Practice Questions
Slide Exam Rotation F 2022 / Block A Slide Exam: 2022-2023
Slide Exam Rotation F 2022
-
Despite being born at term, an eight-hour old infant plots out below the fifth percentile for weight, height and head circumference. On examination, you find an enlarged liver and spleen and the following rash. Laboratory reveals Hematocrit of 33%, platelet count of 40K, 4.3K WBC and a total bilirubin of 10 mg/dl at 4 hours of age. You find no evidence of cataracts or heart disease. The mother is rubella titer positive and RPR negative.

What is the most likely diagnosis?
Congenital CMV- blueberry muffin spots- extra medullary hematopoiesis (can also be seen in rubella, but this mom is rubella immune)In addition to intellectual disability and growth failure, what is the most common serious long-term sequela?
Congenital sensorineural hearing loss -
A two-month-old female infant is brought to the physician for a well-child check. She was seen by one of your partners two weeks ago for "spitting up." She is exclusively breast-fed and is nursing every two to three hours, but "spits up" after half of her feedings and was diagnosed with gastroesophageal reflux. To prevent her from choking, they began placing her in the prone position for sleep. The parents are pleased that the baby is sleeping well since then, but are concerned because the baby's cousin died of SIDS. Because of this concern she sleeps in a bassinet in the parents' room.

What is the most appropriate recommendation regarding sleep to give these parents?
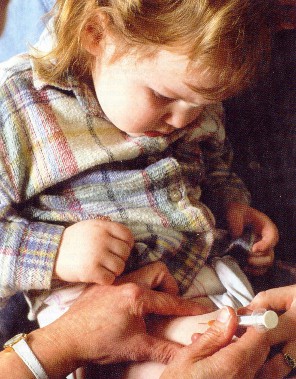
A – alone, B - on their back, C – in their own crib (or sleeping space)Name one thing that's wrong with this picture.
Blanket, lovey, on her side, spit up mat -
An 8 year-old boy with a sore throat developed a widespread fine red sandpaper-like eruption with bright red cheeks, circumoral pallor, and the following oropharyngeal finding. Three weeks later he was admitted to the hospital with marked hypertension and hematuria.


What was the most likely diagnosis three weeks ago?
Strep pharyngitisWhat is the most likely diagnosis now?
PSGNWhat would have been the best therapy three weeks ago?
Penicillin, amoxicillin, or bicillin -
A 6-year-old unimmunized boy presented to the emergency department with fever of 102 F, a barky cough and stridor. The examination shows a RR of 50 bpm with an oxygen saturation of 95% while breathing room air, marked stridor, moderate substernal retractions, and equal aeration without wheezes or rhonchi. Patient is started on nebulized racemic epinephrine but becomes more toxic appearing and drooling. His respirations increase to 75 bpm and he becomes sleepy.
What is the most likely diagnosis?
EpiglottitisWhat is the best action to take at this point?
Intubation by a trained professional (Peds EM, ENT, Anesthesia, PICU) -
A 6-week-old infant is brought to your clinic with a swollen left thigh. The baby has been irritable for the last two days especially with diaper changes. You obtain the following radiograph.

What is the most likely diagnosis/etiology?
Femur fracture – likely inflicted injury (child abuse) but also consider OIIn addition to appropriate medical therapy, what else needs to be done at this point?
Notify MSW, CPS (DCS), law enforcement -
A 16-year-old boy is brought to the physician for complaints of recurrent abdominal pain over the last six months. The pain has been waking him at night, but is vague and hard for him to describe. He reports recurrent diarrhea associated with the pains, and has noted blood in his stools. Review of the chart shows that he has lost 10 pounds since his last visit six months ago. Temperature is 38.2 C, heart rate is 114 bpm, respiratory rate is 24 bpm. Height and weight are at the 10th and 3rd percentiles, respectively. On physical examination there is mild abdominal distention and tenderness localized to the right lower quadrant without rebound. You obtain the following laboratory.
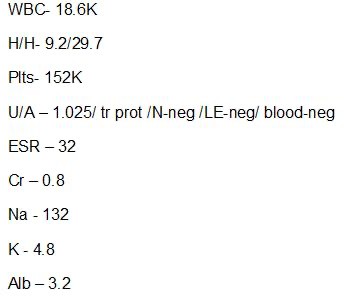
What is the most likely diagnosis?
IBD, likely Crohn’sWhat is the best test to make the diagnosis?
EGD and colonoscopy (must do both to determine extent of disease) -
A 15-yo young woman presents to the ED with 1 day of progressively worsening chest pain. She reports fever and URI symptoms one week ago. Today while in school, she developed sharp chest pain and dyspnea when walking to classes. In the ED, she appears anxious and diaphoretic. T 37.6, HR 120, RR 25, BP 110/70, SpO2 95% on RA. On exam, she is leaning forward on the exam table. Heart rate is tachycardic but regular. You hear an abnormal heart sound but are unsure of what it is, but there is no murmur. Lungs are clear. Abdomen is soft. Her chest pain is not reproducible on exam. Due to her chest pain, you obtain the following EKG.
What is the most likely diagnosis?
PericarditisName one classic ECG finding for this diagnosis.
Diffuse ST elevation
PR depression
Diffuse T wave inversion -
A 5-year-old boy is brought to your office because his mother has noted that his shoes have been getting progressively tighter for the past 2 weeks. This morning, the mother thought that his face, abdomen and legs also looked swollen. On examination, his heart rate is 90 beats/minute, his respiratory rate is 18 breaths/min, and his blood pressure is 105/65 mm/Hg. There is evidence of periorbital and pedal edema.

What is the most likely diagnosis? Be specific.
Nephrotic syndrome, specifically minimal change diseaseWhat would be the best initial therapy?
Steroids -
A 4-year-old girl has been limping for the past 24 hours. Her mother is concerned that she injured her right leg while jumping off her bed 2 days ago. She recently had a viral upper respiratory infection associated with congestion and a low-grade fever but has been well for the past week. She was active until yesterday afternoon. She is afebrile and appears well, except for a pronounced limp on her right leg. She has no rash, joint swelling, or erythema. Passive movement of the right leg through the prone internal rotation maneuver (shown) causes pain in the right hip. Active range of motion of the right hip is reduced.

What is the most likely diagnosis?
Transient synovitisWhat would be the best means of making the diagnosis?
What would be the best therapy?
Clinical- can rule out septic joint by history and physical alone.
If there was concern for septic joint, then would obtain CBC, ESR, CRP first.
Hip ultrasound and xray next.
NSAID's, rest -
A two-year-old girl is brought to her physician for clumsiness. Her parents have noticed that over the past two weeks she has become clumsier and for the past two days has had difficulty walking and sitting without support. They have also noticed episodic, involuntary jerking movements of her arms and legs in the past few days. She has previously been healthy, has had no recent illnesses, and has not had a fever. She has had no nausea or vomiting. Physical examination shows an awake and alert girl. Her temperature is 37.3 C, heart rate is 120 bpm, respiratory rate is 22 bpm and blood pressure 88/62 mmHg. Neurological examination shows erratic, conjugate jerking movements of her eyes and normal fundoscopic exam. Strength and tone of his extremities are normal, and deep tendon reflexes of ankle and knee are 2+ bilaterally. She uses her hands to steady herself while sitting and can walk only with assistance with a wide-based unsteady gait.

Which malignancy is most likely to be found?
Neuroblastoma (this is a description of opsoclonus-myoclonus) -
Take a look at the painting titled “The Doctor” (1891) by Luke Fildes. Write a few responses regarding your observations. If you’re having trouble getting started: Can you spot the parents in the background- what response is father vs mother having? Is the child getting better or worse? Is the doctor thinking about how he will beat this disease or is he beaten and perplexed, or maybe he's none of these? What do you make of the lighting in the painting- what is it saying? What is Fildes saying about medicine or sick people in this painting?

Block A Slide Exam: 2022-2023
-
You are examining a four-day-old boy who is brought in because of an elevated transcutaneous bilirubin found by the home health nurse. He was born at 39 weeks and weighed 2.9 kg at birth. He is having two to three wet diapers per day, and the mother feels he is a little sleepy. He is scheduled to have his otoacoustic exam repeated as he failed it in the nursery. You note microcephaly and hepatosplenomegaly on your physical exam. Blood test shows direct hyperbilirubinemia.

What is the most likely diagnosis?
CMV (congenital)What is the best test to make the diagnosis?
Detection in urine or saliva CMV (viral culture, Raid culture (shell vial), or PCR) -
A twelve-month-old child is brought to your office for well child check. Assuming she received all previous vaccines on time, name at least 3 vaccinations she should receive today.
Any 3 of the following will be considered acceptable:
Hep A
Hib PCV13 MMR
VaricellaFlu if in season and have not already had 2 doses
(DTaP usually given at 15mo)
-
Jennifer, a 4 y/o girl, was seen in the outpatient department for a sore throat, headache, runny nose, cough, and fever for the past 2 days. Her mother reported that another physician had mentioned the presence of a heart murmur on several occasions but had explained that it was not a problem.
On physical exam, her temperature was 102F. Ht and Wt- 50%ile. She had clear rhinorrhea and her throat appeared erythematous. A heart murmur was noted as grade II/VI vibratory (musical) short systolic ejection murmur heard best over the left midsternal and lower sternal border, without radiation. The murmur was best heard when the patient was supine and virtually disappeared when she was upright.

What is the most likely cause of Jennifer's murmur?
Still’s Murmur with a viral URIWhat is the best means to make the diagnosis?
ClinicalFor an example:
Go to Up to Date - under Approach to infant or child with a cardiac murmur, under movies, under innocent still murmur
-
A 17-yo girl is brought to the emergency room with a 5-day history of malaise, fatigue, left and right upper quadrant abdominal pain and two days of painful cervical adenopathy. She was seen by her pediatrician two days before this visit where lab work included a BMP, rapid strep antigen, rapid influenza A&B antigen and a monospot test all of which were negative. The patient experienced severe odynophagia resulting in dehydration and decreased urinary output. Physical exam revealed dehydration, right and left upper quadrant abdominal tenderness, no hepatosplenomegaly, but marked cervical adenopathy. Laboratory included total bilirubin of 2.1, AST 450, ALT 760, UA specific gravity 1.025.

What is the most likely diagnosis?
Infectious MononucleosisWhat is the best test to make the diagnosis?
EBV titers (Monospot is a good test for patients > 10yo and if they have had symptoms for at least 1 week; not specific but sensitive in this population. It is not a great test for younger kids or in patients with symptoms for less than a week)Clinical pearl from Up to Date:
Although they are nonspecific, in the appropriate clinical setting, heterophile antibodies perform well. However, they can be insensitive, especially in some scenarios. As examples:
-
Early infection – The false-negative rates are highest during the beginning of clinical symptoms (25 percent in the first week; 5 to 10 percent in the second week, 5 percent in the third week) [100]. In patients with a compatible syndrome and negative heterophile antibodies, the test can be repeated if the patient is early in his/her clinical illness. Alternatively (or in addition), EBV-specific antibodies can be ordered. (See 'EBV-specific antibodies' below and 'EBV-negative mononucleosis' below.)
-
Young children – Heterophile antibody tests are often negative in infants and children less than four years of age; thus, EBV-specific serologies are generally favored for diagnosing acute EBV infection in young children [108-112]. (See 'EBV-specific antibodies' below.)
-
-
A 6-month-old boy is brought to your office with a one-week history of cough. It started off as a bad cold, but instead of slowly improving, became progressively worse over the week. Mom is also coughing a good deal. The baby has hours that are symptom free with episodes of coughing so bad that he throws up, leaving him weak, fatigued and gasping for air. On exam, you note petechiae on his face and the following eye findings.

What is the most likely diagnosis?
PertussisWhat would be the best means of making the diagnosis?
Bordetella PCR of nasopharynx (Cx pertussis from post. Nasopharynx also acceptable but practically no longer done) -
You are seeing a 10-month-old in your office for the first time for a well child check. The child was born by C-section for breech presentation without complication and has had no hospitalizations or surgery. She has had three sets of immunizations. Her exam is unremarkable except for uneven height of her knees (positive Galeazzi sign) and limited abduction of the right leg.

What is the most likely diagnosis?
Developmental Dysplasia of the HipWhat is the best means to make the diagnosis? (Hint: looks at the child’s age)
Hip x-ray over 6 mos of age. (if the child is less than 4 mo, then US is the test of choice) -
You are seeing a small male for a routine 3-year-old check-up. During the physical exam, you discover a firm, nontender, nonmobile mass in the left upper quadrant of the abdomen.
CBC shows slight lymphocytosis and thrombocytosis. CT scan (shown) shows a large, calcified mass originating from the left adrenal gland. The mass crosses the midline displacing the spleen and left kidney. Chest CT was normal.

What is the most likely diagnosis?
NeuroblastomaWhat additional test can help you make the diagnosis?
24 hr urine catecholamines (VMA, HVA); can also do spot urine catecholamines while awaiting 24hr results. OR Biopsy for diagnosis and staging -
A 6-week-old infant is brought to your clinic with a swollen left thigh. The baby has been irritable for the last two days especially with diaper changes. You obtain the following radiograph. After gathering a history from the caretakers, there is no known mechanism to explain the injury.

What other radiographic studies are recommended in this context to screen for occult injuries (be specific)?
Skeletal Survey and Head CTIn addition to medical therapy, what else needs to be done at this point?
Notify social work, CPS (DCS), and law enforcement. Call CPS must be included to get credit. -
A 18-month-old female comes to your clinic because of diarrhea and poor weight gain. Her mother noted her increased irritability; infrequent loose, foul-smelling stools; and lack of weight gain over the past 2 months. Previously she had been a healthy toddler.
At birth, she weighed 8lbs 2 oz and initially had no problems gaining weight. The family feeds her regular table foods and to add calories, they have started including a flour-lard gravy in most of her foods, but this hasn't helped to increase his weight.
On exam, the child appears well developed but poorly nourished and acts whiny and irritable. You also note herpetiform clusters of vesicles on an erythematous, edematous base with crusts on the upper back and shoulder. (see image). Her weight is at the 2%tile, while linear and head circumference remain at the 50 %ile. The CBC was normal.

What is the most likely diagnosis? (be specific)
FTT due to celiac disease (must include celiac disease)
The rash is dermatitis herpetiformis which is associated with celiac diseaseWhat is the best therapy?
gluten free diet forever -
A 10-year-old boy is brought to the physician with a chief complaint of "funny" colored urine. It has been darker (see picture) in the last few days, but he otherwise feels fine with no complaint of dysuria, frequency, or urgency. He has no significant past illnesses but was seen in an urgent care clinic three weeks ago with a sore throat and headache and was treated with azithromycin for five days. He has been noted to have increased thirst for the last week. Vitals are significant for mild hypertension. Analysis of his urine shows large blood on urine dipstick and too numerous to count red blood cells on microscopy. There was no protein, glucose, ketones, nitrites, or leukocyte esterase on the urine analysis.

What is the most likely diagnosis?
Post-streptococcal glomerulonephritisWhat is the appropriate treatment?
Salt and water restriction, antihypertensives, loop diuretics, dialysis if severe hyperkalemia or uremia; can treat with penicillin/amoxicillin for past Strep too. Any of these answers will be accepted. - Reflect on The Pediatrician. What does this piece of art say about the profession? If you need help getting started,
here are some suggested questions to consider: What is the significance of the baby
angels in the clouds? Why are there animals in the painting? What do or don’t you like about this representation of the field? There
is no wrong answer.